UNAIDS | Asia-Pacific
The Challenge
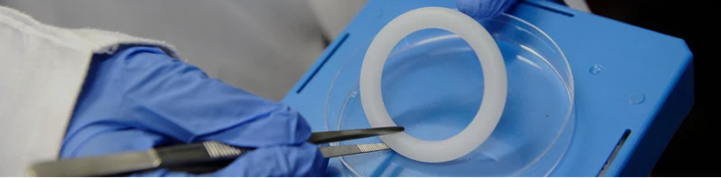
HIV remains a pressing public health challenge across the Asia-Pacific, especially among women at high risk, including female entertainment workers. Despite the urgency, female-initiated prevention methods remain limited. The Dapivirine Vaginal Ring (DVR), a discreet, monthly HIV prevention option, was recently endorsed by WHO as part of the HIV prevention toolkit. Yet its acceptability and feasibility within Asian contexts had not been assessed. UNAIDS and WHO commissioned ThinkPlace to explore the potential for introducing the DVR in Cambodia, Indonesia, Papua New Guinea, and the Philippines – focusing on both demand-side (acceptability) and supply-side (feasibility) perspectives.
Our Response
We conducted a multi-country qualitative study engaging entertainment workers, healthcare providers, community-based organizations, and government stakeholders. Our research aimed to understand the perceived value of the DVR, potential barriers to its use, and the readiness of health systems to introduce it. Across all four countries, entertainment workers expressed a strong willingness to use the DVR, highlighting its autonomy and discretion. They emphasized the importance of accessing it through decentralized, community-based health services. Healthcare providers also welcomed the DVR as a valuable addition to the prevention toolkit, seeing it as a way to expand choice and accessibility.
The study also surfaced underlying concerns that pointed to broader gaps in sexual and reproductive health literacy. Many women had questions about how the DVR works—whether it could move or get lost inside the body, or whether it would affect sexual activity—reflecting a lack of accessible, accurate information about their own anatomy. Others expressed apprehensions about stigma or partner reactions. These insights underscored the need for clear, culturally sensitive education and low-barrier service delivery models.



Our Impact
To ensure findings could inform national planning, we first delivered country-specific reports synthesizing key insights and tailored recommendations. These were shared through in-country dissemination events with national stakeholders, including government, civil society, and community representatives. These sessions served to validate findings, facilitate localized discussion, and support early engagement around DVR integration.
To build on this momentum, we convened a regional DVR launch in Bangkok, bringing together UNAIDS, government representatives, INGOs, and community-based organizations. The workshop provided a platform to share cross-country learnings, explore future opportunities, and address knowledge gaps among decision-makers. It also served as a forum for technical experts to respond to questions and concerns from policymakers—paving the way for more informed, regionally aligned decision-making on the DVR’s potential introduction.


Conclusion
By placing community voices at the center, this project built a robust foundation for country-level planning and advocacy around DVR. It illustrates the power of human-centered research to shape inclusive health policy and unlock new prevention options for those who need them most